Transcranial Doppler, or TCD, is an ultrasound-based, safe, non-invasive means of dynamically surveying flow velocity and pathologic changes in the large arteries at the base of the brain. These include the middle cerebral arteries (MCAs), anterior cerebral arteries (ACAs), terminal internal carotid arteries (tICAs), posterior cerebral arteries (PCAs), ophthalmic arteries (OAs), intracranial vertebral arteries (VAs) and the basilar artery (BA).
Reasons your provider may order a TCD for you:
- Intracranial artery stenosis
- Carotid stenosis
- Shunting/bubble/patent foramen ovale (PFO)
- Brain emboli
- Dizzy/vertebrobasilar insufficiency
- Autonomic dysfunction
What you should know:
- TCD is an ultrasound-based diagnostic
- Ultrasound is not a form of ionizing radiation like XRays or CT scans
- TCD listens to blood flow in the brain
- TCD is completely noninvasive*
*if you are having a TCD bubble study you will have an IV placed, but the ultrasound is noninvasive
Where is TCD performed?
Your TCD will be performed in the University Clinical Health Neurology Clinic, 1331 Union Avenue, Suite 1145 Memphis, TN 38104. Clinic Phone: 901-866-8811
How long will it take?
Anywhere from 30-90 minutes depending on the studies ordered. We can take breaks as needed. If your provider asked for a protocol with routine and monitoring studies then it will be at the longer end of that range. Check which protocol your provider ordered and see “What types of TCD studies are there?” for more details. If your doctor also ordered a CUS that will also take some time and you can get more information on that here.
What should I expect?
Arrive at the University Clinic Health clinic 15 minutes before your scheduled time so you can use the restroom and get comfortable before your procedure. You will be brought to the procedure room and made comfortable on an examination table. We try to keep still and quiet for the examination, as the device can pick up our movements and sounds, but we can easily take breaks as needed since it is difficult to lie still and quiet for long periods of time. Ultrasound gel is used for this study, and it gets on our skin and hair, but is easily washable and nontoxic. The sonographer (e.g., person doing the test) will hold the plastic probe next to your ear, below your eyebrow, under your chin and on the back of your neck to listen to brain arteries. Depending on the test ordered, you may have a headband applied that holds these plastic probes in place for longer periods of listening. Once the study is done, the sonographer will help you wipe up the ultrasound gel and then you can go home. Your results will be made available to you as soon as possible.
- You may be asked to take off your glasses because we typically listen next to the ear and the glasses can get in the way.
- You may wish to wear a tshirt or something that stretches at the neck so we can avoid getting gel on your clothing
What types of TCD studies are there?
TCD studies may be simple “routine” studies where we hold the probe on the side of the head and listen, or more complicated “monitoring” studies that involve the use of a headband holding the probes in place and we listen to arteries over a longer period of time.
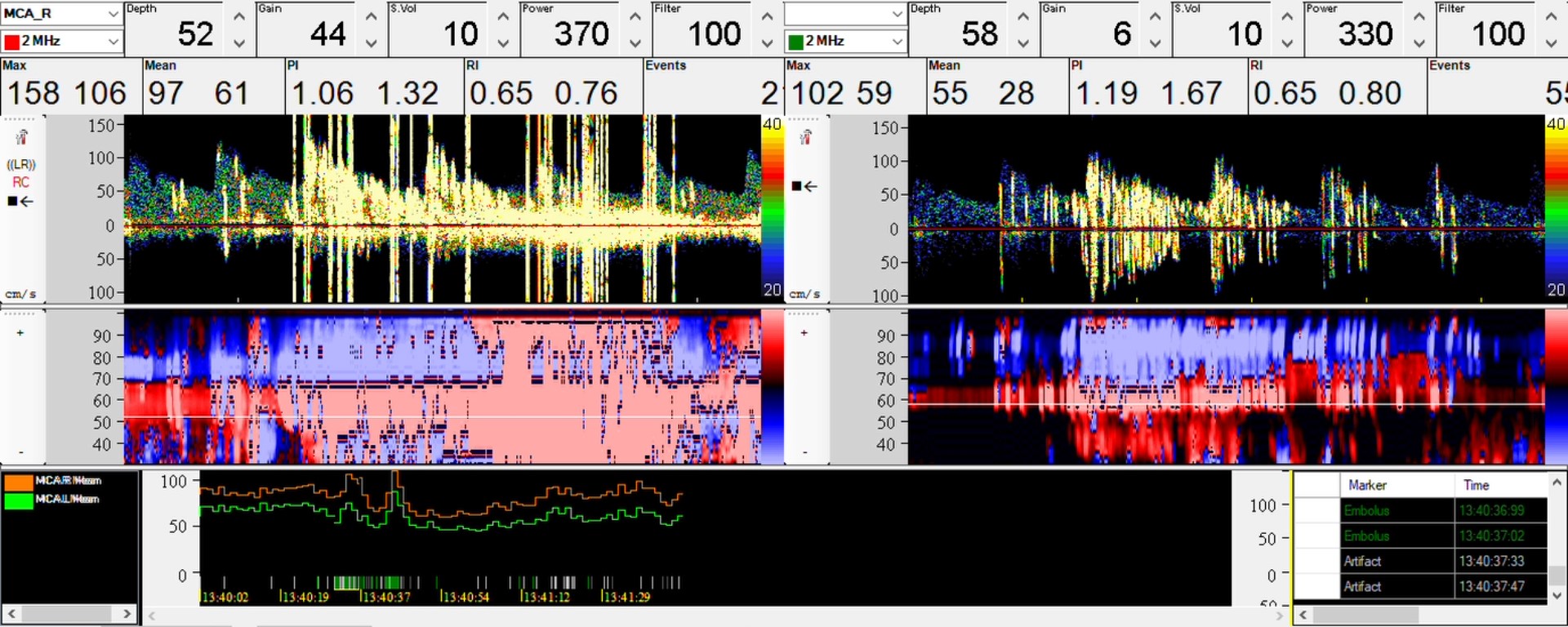
- One type of monitoring study involves applying the headband and simply listening over time if your provider is worried that small bits, called “microemboli,” are being sent toward your brain.
- We can also monitor how healthy the blood vessels in the brain are by having you briefly hold your breath to see how they react. We are listening for “vasomotor reactivity.”
- Another type of monitoring study involves the placement of an IV and injection of a mix of saline and a tiny amount of air – a “bubble study” – and to listen for those bubbles we injected to see if they go from vein-to-brain. This study is done routinely with TCD and echocardiography and is safe.
Your provider will let you know exactly which studies you should expect by indicating which of these protocols they think you should have:
- Intracranial artery stenosis
- Routine study + monitoring (breath holding and emboli)
- Carotid stenosis
- Routine study + monitoring (breath holding and emboli)
- Shunting/bubble/PFO
- Routine study + monitoring (bubble study)
- Brain emboli
- Routine study + monitoring (emboli)
- Dizzy/vertebrobasilar insufficiency
- Routine study + monitoring (breath holding, head turning)
- Autonomic dysfunction
- Routine study + monitoring (breath holding)
